Spore-forming microorganisms (bacteria and fungi) are the most challenging microorganisms for a facility’s contamination control programme. This is because:
- Spores are difficult to destroy using most cleaning and disinfection processes.
- Bacterial endospores are resistant to desiccation, temperature, starvation, ultraviolet and gamma radiation, and chemical disinfectants.
- Spores can be spread over considerable distances, e.g., transferred via trolley wheels, harboured in cardboard packaging, etc. or through fungal dispersal.
- When the environmental conditions are suitable, spores will germinate.
Even with the best designed cleanrooms and supporting procedures, sporicidal disinfection remains a critical component of the contamination control programme. There is an important choice for the cleanroom user to make in terms of the type of sporicide to be selected.
Sporicidal agents
Disinfectants are designed to reduce a population of microorganisms on a surface down to a safe level (microbiocidal action). Many disinfectants, while effective against vegetative cells, are not sporicidal. To kill bacterial and fungal spores the cleanroom needs to deploy a special class of disinfectant called a sporicide.
The majority of sporicides available are either chlorine derived, like sodium hypochlorite, chloramine, chlorine dioxide, and hypochlorous acid; or hydrogen peroxide, peracetic acid, or a blend of the two chemicals. These disinfectants display multiple modes of action against microorganisms, such as penetrating the cell wall, disrupting the cytoplasmic membrane or by destroying intracellular components.
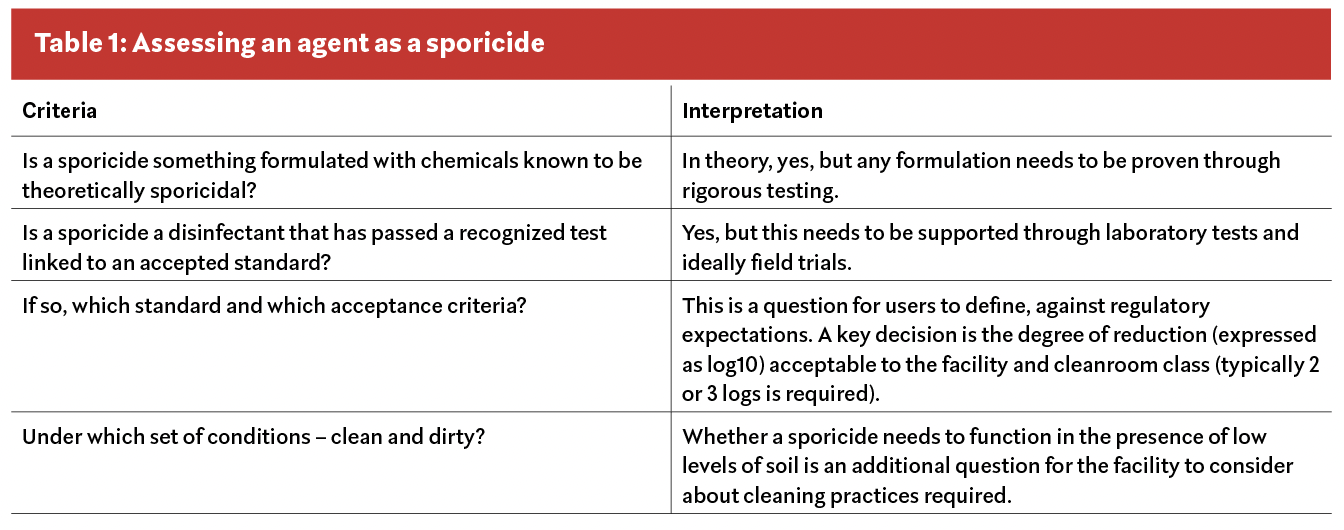
As well as the chemicals and their formulation there are other criteria that contributes to making something a sporicide, Table 1 sets out some basic requirements.
What makes an optimal sporicide?
When the cleanroom manager is considering which sporicidal agent to select, several factors need to be evaluated. The section below reviews these factors, with a summary provided in Table 2 .
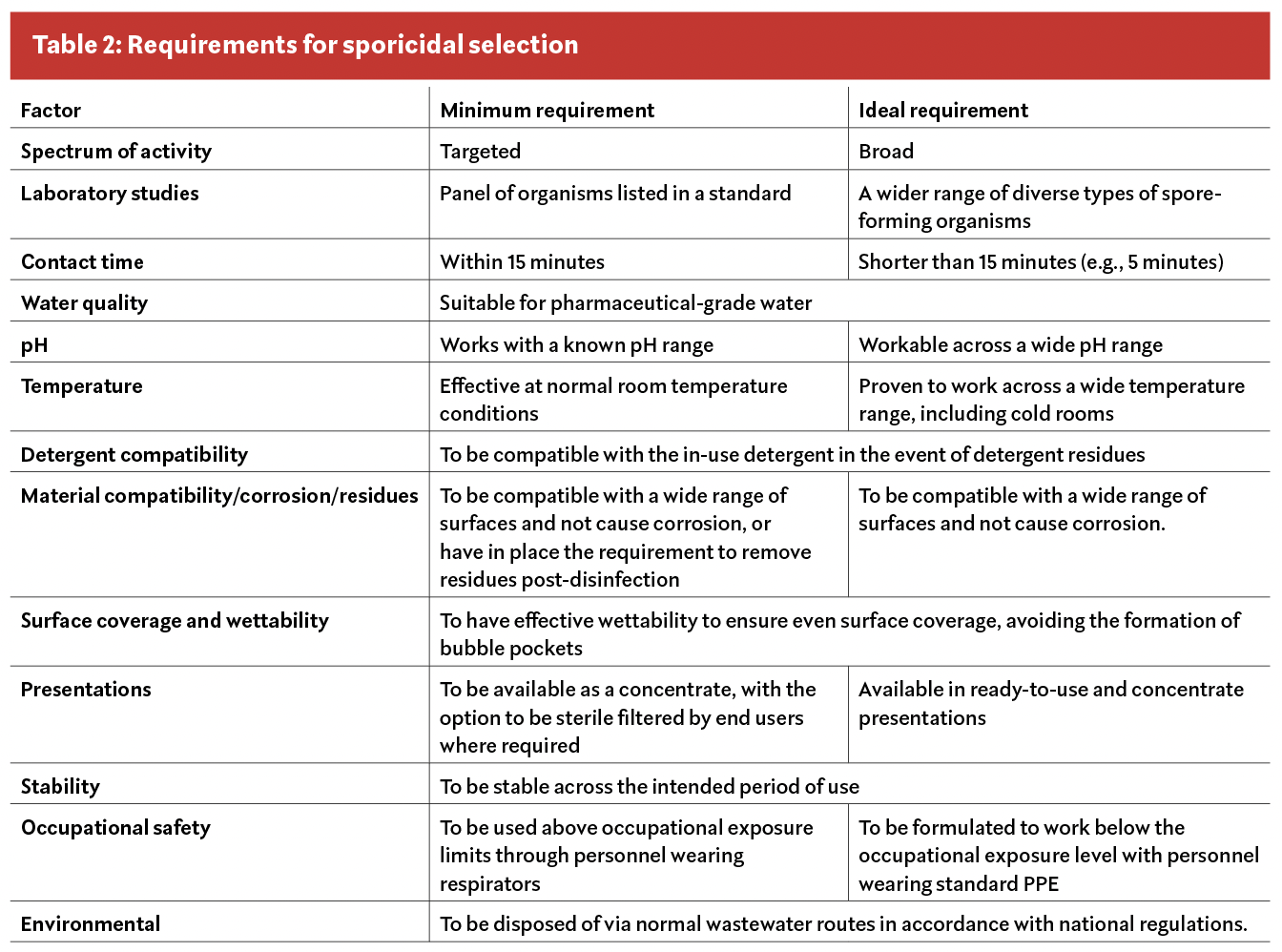
Spectrum of activity: This refers to the ability of the disinfectant to kill distinct types of microorganisms and microorganisms which are in different physiological states. In the case of sporicides, this is a necessary indication that the product can kill both bacterial and fungal spores from several representative species.

