Having to visit a hospital is usually not a particularly pleasant event. Acquiring an infection during the stay makes it even worse. Nowadays, the so-called hospital-acquired infections (HAIs) are on a seriously high level. In Germany, HAIs cause about twice to three times as many deaths as traffic accidents.
Around 4,500 people die each year after suffering from a post-operative wound infection (POI) caused by bacteria entering the open wound during the operation. Different types of surgery have varying risks of infection.
Another issue that is often forgotten is the spread of surgical smoke. In electro and laser surgery as well as in ultrasound applications, the tissue is separated or scabbed, and bleeding is stopped using heat or ultrasound. Thus, surgical smoke is released as a by-product made of water vapour, gaseous and molecular pollutants and particulate matter. Besides unpleasant odours, they pose a health risk to the medical staff.
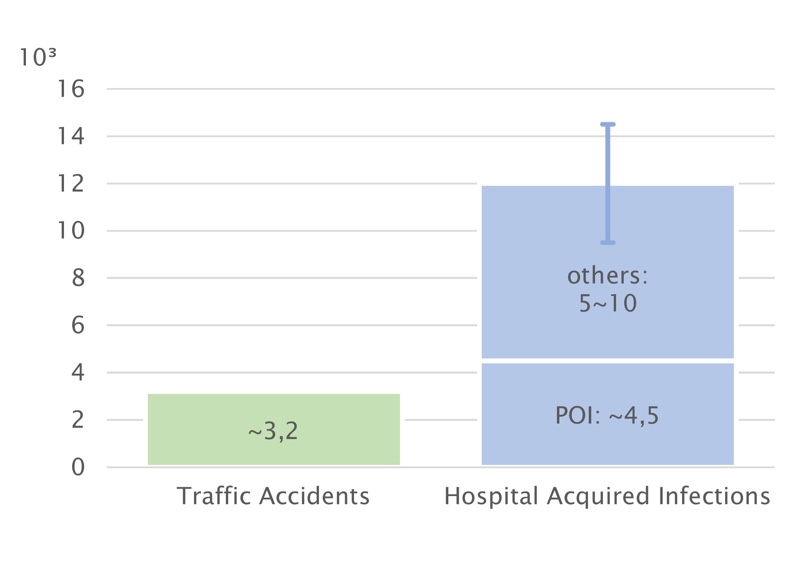
Figure 1: Death cases in Germany by HAI and traffic accidents
Currently, there is much discussion on the pros and cons of different ventilation systems in operating rooms. Usually, unidirectional airflow (UAF) is compared to turbulent mixing ventilation (TMV). Many authors state that UAF is superior to TMV regarding the observed number of colony-forming units (CFU) in the air or on sedimentation plates.
In publications by Erichsen Andersson et al. (2014), Hansen et al. (2005), Ljungqvist und Reinmüller (2013), Whyte et al. (1982), and others, CFU measurements in operating rooms (ORs) with UAF were compared to measurements in rooms with other ventilation systems, mostly mixing ventilation. Lower numbers of CFU were observed with UAF in each study.
However, rooms with UAF were always equipped with HEPA filters while the others were not. Thus, these studies are not appropriate to state the quality of the airflow patterns, as the boundary conditions differ essentially.
These studies are not appropriate to state the quality of the airflow patterns, as the boundary conditions differ essentially
It seems that currently the wording “unidirectional airflow” implies the use of HEPA filters while “turbulent mixing ventilation” is usually associated with the absence of HEPA filters. Such an assumption is technically unfounded! Comparisons between airflow patterns must be done with the same quality of air filters.
Besides air filtration, there are other crucial boundary conditions when comparing two scenarios, especially the overall air flow rate, equipment inside the OR and the locations and strengths of the contamination sources.
In the project “Energy Efficient Ventilation of Operating Rooms”, funded by the German Federal Ministry for Economic Affairs and Energy, the effect of different indoor airflow patterns on both the infection risk through airborne bacteria and the dispersion of surgical smoke, is investigated under realistic boundary conditions, considering the equipment the personnel’s postures. The research also evaluates the thermal comfort for the personnel and the risk of hypothermia. The investigations are performed experimentally and employing computational fluid dynamics (CFD).
The unique approach in this project is to have a single operating room (OR) laboratory (see Figure 2) that can provide a variety of different ventilation patterns by design. Thus, it is possible to compare them with all other boundary conditions being most realistic and constant.

Figure 2: The operating room research laboratory
The OR laboratory has been equipped with numerous air diffusers for supply and exhaust air. Unidirectional airflow, turbulent mixing ventilation, and stratified displacement ventilation can be realised at the push of a button.
The airflow rate of each diffuser can be individually controlled. Additional supply and exhaust ports allow for the installation of locally arranged air diffusers.
Ventilation requirements in the OR
Besides the direct transfer by contact, the air acts as a carrier (airborne particles), or as a medium (larger particles) for pathogens. POI may occur as the result of a pathogen transferred to an open wound.
Infectious germs may appear as airborne particles, or capsulated in droplets, or on skin scales. Droplets and skin scales are not airborne and thus sink regardless of the ventilation. However, droplets may become airborne, if the water part evaporates.
It can be assumed that the operating personnel are responsible for about 80% of all contamination in an OR; the head being the main source and they are also the primary origin of germs.
The performance of the OR ventilation system and the resulting room airflow can be assessed by a variety of parameters:
- Concentration of airborne microbial contamination (protective effect)
- Thermal comfort and room climate (important for concentration and work performance)
- Spread of surgical smoke (potential health risk for surgical staff)
- Risk of hypothermia (increases the risk of infection)
- Energy efficiency of the ventilation system (a non-health related aspect)
The primary parameter of interest is the protective effect for the critical areas (wound field) against airborne microbial contamination and is also a major focus in the experimental work in the current project.
Experimental methodology
The position and geometry of microbial and heat sources in ORs are decisive factors regarding the spread of contaminants. As mentioned above, bacterial contamination is mostly emitted from the facial region of the personnel in the room. The surgical staff is often in a bent position over the operating table.
A set of customised person simulators was designed for geometry, heat flux and particle emission. Each manikin is wrapped with an electrical resistance wire for heating the surface. The specific heat load ranges from 85 up to 125 W, depending on the position and the assigned activity of each person simulator.
The project worked out a set of five operating arrangements to generalise the results of the experimental measurements. Each setup shall represent one typical operating procedure with high impact of airborne contaminants to the risk of a surgical site infection.
The different types of representatives are:
- Total hip endoprosthesis (Hip-TEP) with a high and low number of present personnel
- Hand operation with a high and low number of present personnel
- Head operation
Figure 3 shows the typical setup for Hip-TEP surgery with staff
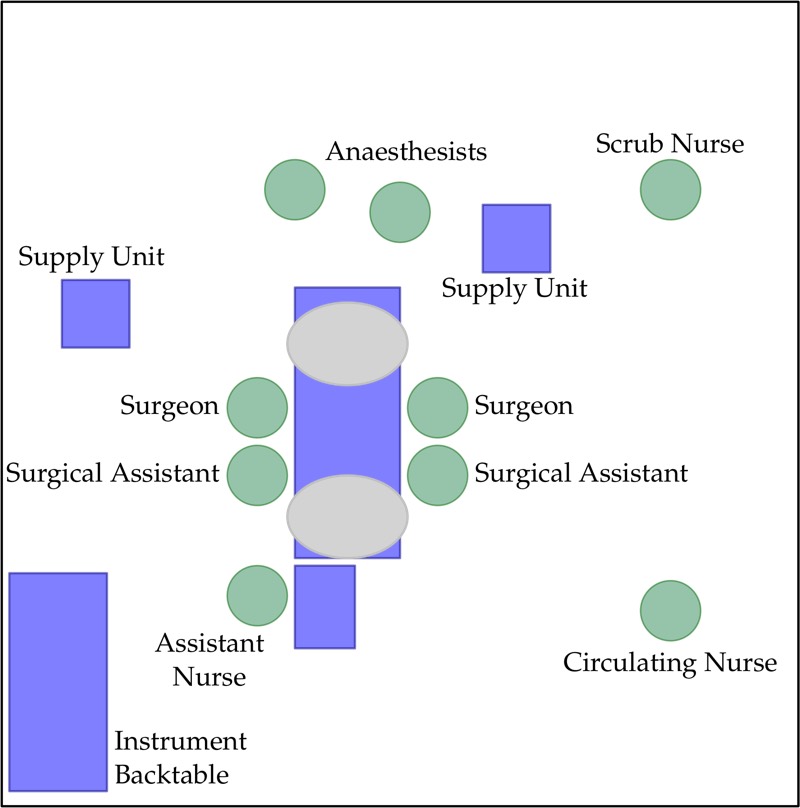
Figure 3: Typical setup for Hip-TEP surgery
Microbial contamination is emitted in the form of saliva droplets or skin flakes from persons in the operating room. These particles contain bacteria that can cause surgical site infections.
The CFU in the room air occur as an agglomeration of several bacteria together with further organic and inorganic material. In the literature, particle sizes of the bacterial infectious agents in ORs are described with a size range of 2-12 µm.
It should be mentioned that especially skin flakes with bacteria adherent to the surface can also form much larger particles. These particles >20 μm deposit quickly by gravitational settling. Particles >1 μm show a different motion behaviour in indoor airflow compared with standard sub-micron particles used for cleanliness tests.
For the reason of experimental reproducibility, it was decided to use an inorganic tracer aerosol as a surrogate for CFUs. However, conventional aerosol generators emit particles mostly around 0.2 to 0.5 μm. A feasible method for application in experimental investigations was developed to produce a tracer aerosol with particles of a size >1 μm. For this purpose, a suspension of solid tracer particles of the appropriate size range in desalinated ultrapure water is nebulised.
The aerosol is released in the facial area of the person simulators and is evaluated at critical points such as the operating table and the instruments table. From the measurement data, a contaminant transfer coefficient can be calculated between each person and the critical measurement points. The transfer coefficient is the ratio of released particles to particles transferred to a certain critical point.
The transfer coefficient is a suitable measure to compare different ventilation schemes with different setups. Lower transfer coefficients indicate higher patient protection and vice versa.
Surgical smoke dispersion
As mentioned above, not only the infection risk is of importance. The research has paved the way for an insight into the surgical smoke problem.
CFD investigations of surgical smoke dispersion show the significant influence of the lamp on the indoor airflow. For a typical surgical setup, the field of smoke concentration released at the wound field is evaluated for TMV and UAF with and without the lamp.
Lowest concentrations (approx. 0) in the personnel’s breathing zone can be achieved using UAF without a lamp and under the assumption of upright standing staff. Concentration values increase significantly by applying the lamp in an unfavourable position, e.g. aligned horizontally above the surgical field. The analysis shows that TMV leads to considerably lower concentrations (see Figure 4).
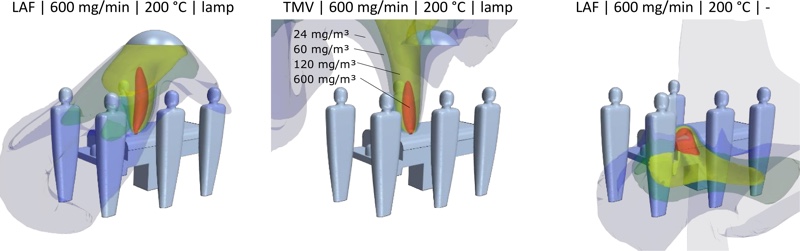
Figure 4: Surfaces of a constant concentration of surgical smoke under different ventilation conditions
This effect is caused by a recirculation area underneath the lamp. As an illustration of that phenomenon, Figure 5 shows the wake visualisation behind a small board in a unidirectional airflow. Within this area, the air exchange is poor, and contaminants released within stay there for a long time.
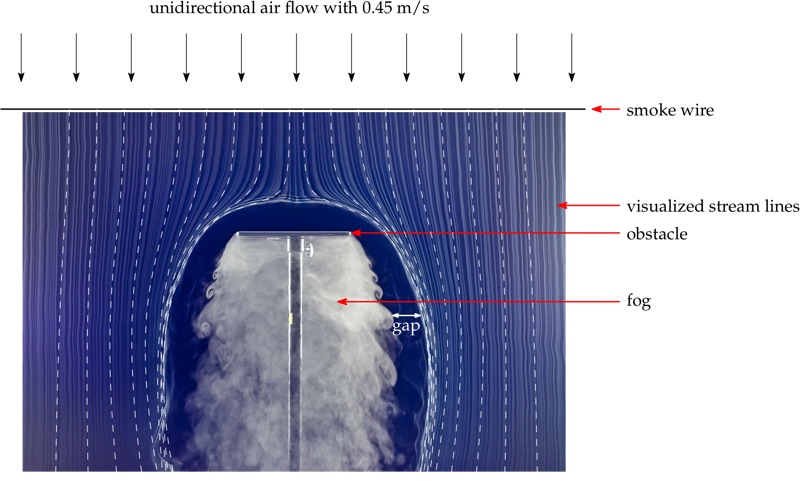
Figure 5: Recirculation area under a flow obstacle in unidirectional airflow
Promising application
As mentioned above, the transfer coefficients will be obtained from the experiments. Based on these numbers, it will be possible to compare the different ventilation patterns on a scientific basis.
It is expected that different ventilation patterns are optimal for different surgical setups. Building upon this fundamental outcome, new ventilation schemes will be developed to provide better performance for specific configurations. These include local ventilation and hybrid ventilation systems.
The investigations will also determine recommendations for different operating room types and requirements based on the experimental and numerical results for the other relevant aspects: smoke concentration, thermal comfort, hypothermia risk, and energy efficiency.
The project is expected for completion in mid-2020.
N.B. This article is featured in the May 2019 issue of Cleanroom Technology. The digital edition is available online.
