Manual cleaning is rarely suitable as a stand-alone process in the cleanroom environment.
There are three elements to consider — the person undertaking the cleaning, the chemical being used and the material or method being used to apply the cleaning process.
At each stage of the process there are opportunities for errors to occur.
In addition, there are various challenges to ensuring that decontamination is properly carried out in a cleanroom or high care environment.
Cleanrooms, bio-cabinets, fume cupboards and operating theatres by their very nature will be complex spaces — some can be substantial in size and others extremely small and confined due to the nature of work that is carried out.
In some of these environments there will be high-risk pathogens to be dealt with and in others lower risk micro-organisms.
However, in all cases there is the universal challenge of how they can be decontaminated quickly, effectively, with suitable equipment and without causing damage to surfaces or sensitive equipment.
At the same time, decontamination needs to be achieved at an affordable cost. There is also the problem of how to decontaminate hard-to-reach areas and how to cleanse the air of airborne viruses.
There have been several studies during 2015 into the efficiencies of manual cleaning.
Dr Tim Boswell at Nottingham University Hospital presented at the Infection Prevention Society (IPS) annual conference in Liverpool, UK and referred to a multi-centre study across 23 acute care hospitals. Defined high-risk objects in patient isolation rooms were marked with UV prior to terminal manual cleaning and the sites were inspected afterwards.
Overall, 49% of the objects or surfaces were not cleaned properly and some of the items which were found still to be contaminated were toilet handles, light switches and door handles.
All of these are perfectly accessible and should have been decontaminated during the terminal clean process.
Manual error will always creep in to these types of situations and that is without even starting to consider what chemicals to use, how they should be used and how they should be applied and with what piece of equipment.
It is commonly accepted that manual cleaning will remove physical debris but it is inefficient at dealing with micro-organisms and hard to reach areas.
There is also evidence to suggest that manual cleaning with a cloth and a biocide solution can actually spread bacteria and cause cross-contamination.
So is there a better method that can complement manual cleaning and which is effective, safe and inexpensive?
This leads to the subject of hydrogen peroxide (H2O2), a well-known, highly tested substance which has proven to be highly effective in killing 99.99% of viruses, bacteria, germs and micro-organisms.
H2O2 can be deployed in a liquid form or using a fogging or spray device to deliver it as a ‘dry mist’. It can therefore be used safely on any surface type including sensitive components, electrics and electronics. In its mist form, it can reach into the most inaccessible areas of a cleanroom or laboratory.
The effectiveness of H2O2 can be further enhanced by the addition of silver ions.
Effective concentration
There has been much debate about what concentration of an H2O2 solution is the most effective.
Health Protection Scotland published a literature review and practice regulations in May 2015 on the subject of H2O2 used for the decontamination of the healthcare environment, and in the publication there were a number of conclusions highlighting that H2O2 vapour (HPV) was as effective or more effective than any of the concentrations of hypochlorite that were reviewed from the studies.
The paper left open the subject of the practical considerations when it comes to the use of HPV to decontaminate in the healthcare environment and this is always a primary consideration due to the number of infectious pathogens and the types of environment and surfaces where they can be found.
Despite detailed scientific evidence to the contrary, a myth persists that concentrations of 30% HPV are required to be effective. However, these levels offer inherent risks to the user and evidence shows that they can cause corrosive damage to surfaces and soft furnishings.
At the IPS conference in 2015, the Nottingham University Hospital NHS Trust presented a study on its use of a H2O2 dry mist system at 5% concentration with silver ions.
The study was launched in 2008 and involved 14 machines across two campuses with the original purpose of the routine terminal disinfection of isolation rooms for C. difficile as well as selective use for outbreaks and at the request of the infection prevention and control team.
In both the table and figure below there is a dramatic difference in the infection rates of C. diff and MRSA after the use of HPV at 5% concentration was introduced.
Figure 1
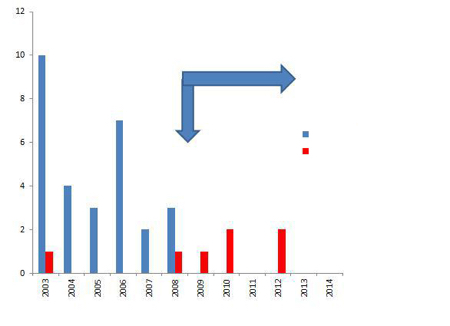
MRSA incidence in burns theatre after decontamination with H2O2. Source: Presentation by Dr Tim Boswell at IPS 2015 annual conference in Liverpool
Table 1: Environmental sampling 2006 versus 2011
| Year | Environment sampled: Health facility for elderly | Percentage of rooms positive for C. diff | Percentage of samples positive for C. diff | C. diff CFU per 10 samples |
|---|---|---|---|---|
| 2006 | Isolation Room* | 100 (8/8) | (24.5 (40/163) | 7.2 |
| Sluice | 100 (2/2) | 20 (8/40) | 5 | |
| Total | 100 (10/10) | 23.6 (48/203) | 6.8 | |
| 2011 | Isolation Room* | 12.5 (1/8) | 0.6 (1/163)1 | 0.06 |
| Sluice | 50 (1/2) | 2.5 (1/40)2 | 0.25 | |
| Total | 20 (2/10) | 1.0 (2/203) | 0.1 |
*Isolation Room cleaned for reoccupation
1. 2006 Ribotypes: 001 , 027, 106
2. 2011 Ribotypes: 005, 037
Source: Staniforth, Vaughan, Boswell. Poster 1953 FIS HIS 2012
The evidence points towards the fact that HPV can provide an excellent solution for decontamination of the cleanroom environment. As shown by the evidence (below, left) the optimal level of concentration is 5%.
At this level there are minimal safety concerns for the user and the environment where it is deployed. The dry mist can reach into any area and as it dissipates shortly after contact it does not produce any surface corrosion and no residue is left behind.
The treatment process can be used in the smallest size of cabinet right up to an entire cleanroom. It is quick, cost effective and can be carried out in as little as 30 minutes so that operational downtime is kept to a minimum.
Sanondaf specialises in infection control and room decontamination using fogging and electrostatic spray devices to deliver H2O2 with silver ions at a concentration of 5%.
The machines are small and highly portable and designed to be used by a single operator. As a disinfection service provider, the company responds to outbreaks or carries out routine maintenance in any type of area that has a requirement to be clear of micro-organism contamination.